This post is part of an ongoing series on how healthcare technology is evolving as autonomy becomes a practical requirement rather than a future aspiration. In the first post, we explored why autonomous decision-making and automation are essential to reducing administrative burden and improving care delivery. In this post, we step back to examine how the broader healthcare stack is reorganizing and why a new platform layer is emerging to support that shift. In future posts, we’ll move from architecture to reality, showing how this execution layer comes to life across real healthcare workflows and intelligent applications. Together, this series reflects how we see the next era of healthcare software taking shape that’s grounded in experience, shaped by market realities, and focused on outcomes over abstraction.
Healthcare is entering a new phase of competition, one defined less by who has the most data or the smartest algorithms, and more by who can reliably turn decisions into action. Over the past decade, health systems invested heavily in systems of record and analytics. Today, those capabilities are widespread. What remains scarce is execution.
This gap has become impossible to ignore. While AI adoption has accelerated across healthcare, the majority of deployments struggle to move beyond pilots. Insights are generated. Alerts are triggered. Tasks are created. But end-to-end outcomes remain elusive. The constraint is no longer intelligence but it’s the absence of a shared system that can coordinate work safely across fragmented workflows, policies, and systems.
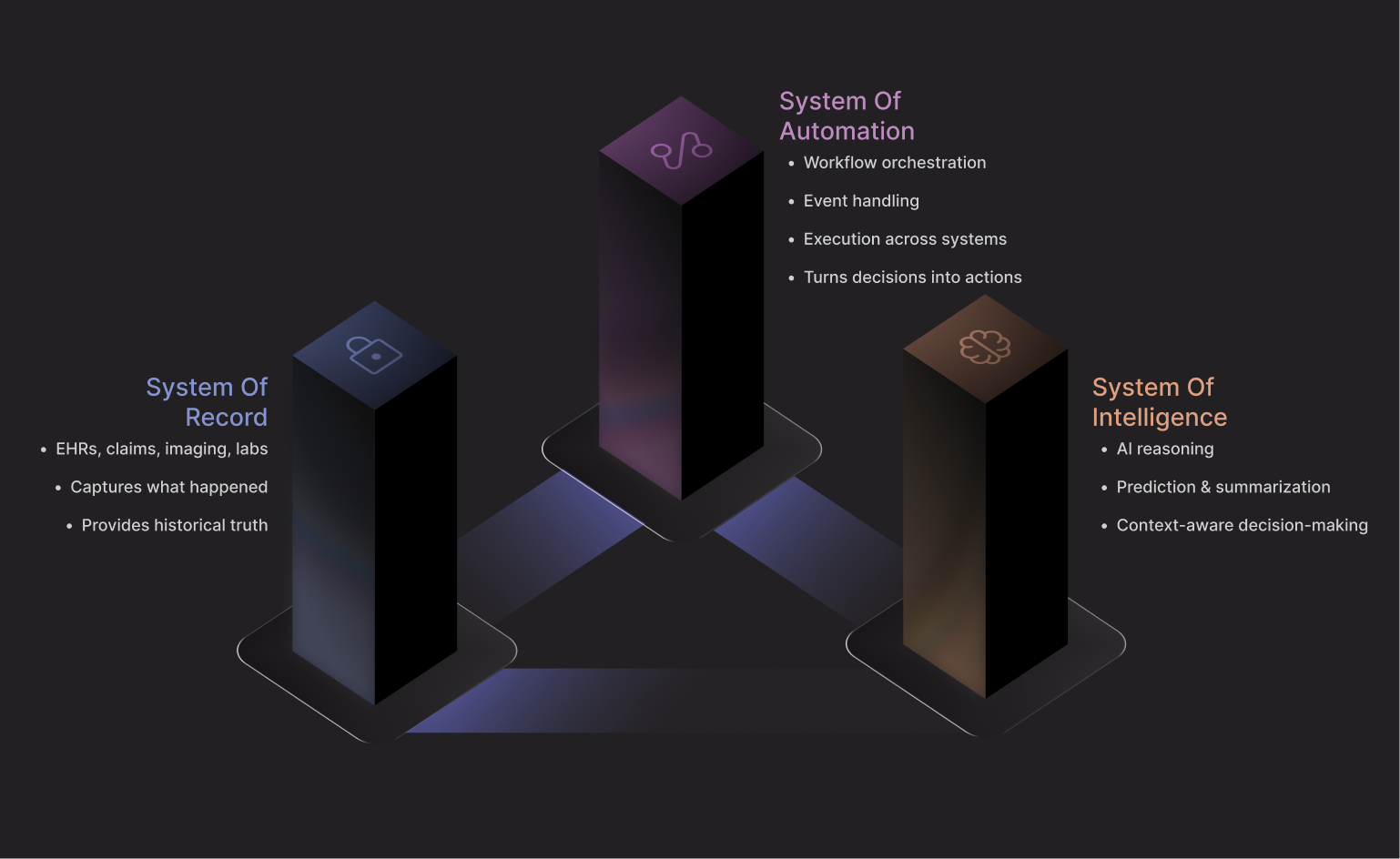
What’s emerging in response is a structural shift in the healthcare technology stack. Alongside systems of record and systems of intelligence, a third category is taking shape: a System of Automation: a platform layer designed to sit between data and action. Not as another application, but as the execution backbone that allows intelligence to operate, governance to be enforced, and work to move across the enterprise. This post explores how that shift is unfolding and why the platform that owns execution is becoming the strategic center of gravity in healthcare.
Why Point Solutions Are Breaking Down
Healthcare didn’t become complex by accident.It became complex by solving workflows one at a time.
- Scheduling tools
- Care management systems.
- Authorization platforms.
- Patient engagement apps.
- Revenue cycle software.
Over time, health systems accumulated dozens and sometimes hundreds of specialized tools. Recent surveys show that more than 60% of health systems now use over 50 unique software solutions, and nearly a quarter manage hundreds. The cost of this complexity isn’t just financial. It shows up as fractured workflows, operational drag, staff burnout, and delayed care. The problem isn’t that tools fail, it’s that they don’t work together.
Fragmentation Is Now the Bottleneck
At a certain point, adding more tools stops increasing capability and starts degrading it. Healthcare has crossed that threshold.This pattern is not unique to healthcare. Other industries have already lived through it.
In financial services, banks once layered fraud tools, risk engines, payments systems, and compliance software on top of one another. Each solved a narrow problem well. Collectively, they created brittle operations where money could move faster than decisions. The response was the emergence of transaction platforms that could coordinate risk, policy, and execution in real time.
Logistics followed a similar arc. Shipping companies didn’t win by adding more route-optimization tools or warehouse systems. They won by building orchestration layers that could see inventory, demand, weather, labor, and routing together and act across them instantly.
Healthcare is at a similar inflection point. Every new point solution adds another integration, another workflow, another place where things can quietly break. Even with modern interoperability standards, real-world healthcare integrations still require custom mapping, constant maintenance, and human supervision. As the tool count grows, moving anything end-to-end, from insight to outcome, becomes cost and resource-intensive, not easier. From our experience, execution slows. Risk accumulates. People step in to compensate.
What’s striking is that nothing is technically “broken.” Alerts fire. Tasks are generated. Dashboards update. Yet outcomes stall because no single system owns the full arc from signal to action to resolution, and this is how complexity becomes the bottleneck.
Why Autonomy Collapses Without an Execution Layer
For a system to operate autonomously, data must be standardized into interoperable products within a unified operational backbone, enabling workflows to trigger across domains, policies to be applied consistently, and exceptions to be escalated safely. When those responsibilities are spread across dozens of applications, autonomy collapses into coordination, and people become the glue holding workflows together.
In other industries, this lesson was learned the hard way. Specifically in cloud computing. Early enterprises layered monitoring tools, deployment tools, security tools, and cost-management tools on top of one another. Automation remained elusive until platforms emerged that could coordinate infrastructure state, policy enforcement, and execution in a single control plane. Only then did “autonomous” infrastructure become possible.
Healthcare hasn’t yet built that control plane. Currently, point solutions aren’t failing, but they’re simply reaching their natural ceiling. They generate insight and activity, but they don’t own execution, which is what determines outcomes.That realization forces a deeper question: if execution doesn’t belong inside any one application, where does it belong?
The Platform Shift: Sitting Between Data and Action
Healthcare is now experiencing the same inflection point other complex industries faced years earlier.Data is abundant. Intelligence is improving. Health systems are awash in clinical records, claims, operational metrics, and patient signals. Intelligence is advancing just as quickly—predictive models, copilots, and generative tools are now commonplace. And yet, the hardest part remains unchanged: reliably turning insight into action inside real workflows.
When that gap persists, organizations don’t fix it by adding more applications. They fix it by changing the architecture.It doesn’t start by replacing existing systems of record or intelligence tools, but by introducing a layer that sits between them and absorbing fragmentation, coordinating execution, enforcing rules, and closing the loop from decision to outcome.
We’ve seen this pattern before. In e-commerce, marketplaces didn’t replace payment processors, inventory systems, or fraud engines., they orchestrated them. In enterprise IT, workflow platforms didn’t replace databases or analytics; they became the connective tissue that allowed data and logic to move safely across systems. In finance, trading platforms didn’t outgrow risk engines, they centralized execution so risk could be enforced in real time.
The next generation of healthcare leaders will not be defined by who stores the most data or trains the most sophisticated models. Those capabilities are rapidly commoditizing. They will be defined by who can consistently move from signal to action across the full care and operational continuum, without breaking workflows, increasing risk, or burning out staff.
This is where the System of Automation becomes strategic.
A true automation platform does not compete with systems of record; it integrates with them. It does not replace intelligence; it gives intelligence somewhere to operate. It orchestrates workflows across clinical, payer, operational, and patient-facing domains, carrying context with them instead of forcing humans to reassemble it at every handoff.
When that layer exists, several things change at once. Intelligence no longer needs to worry about how work gets done. Execution becomes safer because it is observable, auditable, and policy-driven. And innovation accelerates because new models and tools don’t require bespoke plumbing or one-off integrations every time.At that point, autonomy stops being an aspiration. It becomes an architectural property of the system itself.
Why Intelligence Alone Won’t Create Advantage
Artificial intelligence is advancing at an extraordinary pace. Models are becoming cheaper, more accurate, and more widely available. Within a few years, access to high-quality prediction, classification, and reasoning will no longer differentiate healthcare organizations.
Other industries have already seen this dynamic.
In marketing, recommendation algorithms quickly became table stakes. Advantage shifted to platforms that could execute personalization across channels in real time. In finance, risk models became ubiquitous; differentiation moved to systems that could act on those models instantly and compliantly.
Healthcare will have to follow the same path. The real question is no longer whether a system can produce an insight. It’s what happens next. Does that insight trigger the right workflow? Apply the right policy? Reach the right person? Execute in the right system? Get logged, audited, and governed? Or does it become just another notification that someone has to chase down?
How the Market Needs to Reorganize
From our experience, the healthcare technology market needs to reorganize structurally and what’s emerging is a three-part ecosystem of interaction.
Systems of Record: Holding the Truth
EHRs, claims platforms, and administrative systems capture the clinical and operational history of care. They remain essential infrastructure for compliance, continuity, and trust.
But systems of record are not designed to execute.
- They document.
- They persist state.
- They do not decide or act.
That limitation isn’t a failure. It’s simply their role.
Systems of Intelligence: Generating Insight
On top of those records sits a fast-growing layer of intelligence: predictive models, copilots, analytics engines, and AI-driven applications. These systems interpret data, identify patterns, and surface recommendations.
They answer important questions: what might matter, what could happen next, and where risk exists. But in most cases, they stop there.
Automation Platforms: Where Outcomes Are Made
The missing piece and the layer the market is now converging around is automation.
Automation platforms sit between data and action. They don’t replace systems of record or intelligence tools, they connect them. They orchestrate workflows across clinical, payer, operational, and patient-facing systems. They enforce policies, coordinate work, and close loops that would otherwise depend on human glue.
Many health systems now operate dozens, sometimes hundreds, of disconnected tools. Each works in isolation. Together, they slow execution, increase risk, and push coordination onto people. That fragmentation isn’t a tooling problem. It’s an architectural one.
Why This Matters Across the Healthcare Ecosystem
This is where healthcare’s next competitive advantage, but more importantly, how and where care is delivered will be decided. Providers will use it to reduce administrative drag and keep patients from falling through the cracks. Payers will use it to streamline authorization and manage risk without increasing friction. Life sciences organizations will use it to support adherence, evidence generation, and patient engagement at scale.
The use cases vary. The underlying requirement does not.All of them must coordinate decisions across clinical systems, payer systems, patient channels, and operational workflows. None of that can happen inside a single application.
That’s why autonomy ultimately requires a shared execution layer: a horizontal platform where intelligence from many sources can operate, governance is enforced by default, and workflows close end to end. This is not a provider platform or a payer platform or a life sciences platform. It’s a healthcare execution platform.
The Strategic Bet
Healthcare will continue to produce better EHRs, smarter AI models, and more specialized applications. The most valuable healthcare companies will not be the ones that store the most data or train the most models. They will be the ones that can reliably carry decisions into the real world, across systems, teams, and workflows because that’s where care actually happens and that’s where outcomes are ultimately determined.
As data and intelligence become easier to access, execution becomes harder to replicate. That’s why the strategic center of healthcare software is shifting away from records and toward platforms that coordinate, govern, and execute work at scale.
What Comes Next
Healthcare is at a turning point where the architecture is shifting, market is reorganizing and where execution has become the center of gravity. Which raises the next question: what does a real System of Automation look like in practice?
- How does it connect to existing systems?
- How does it enforce governance?
- How does it allow intelligence to operate safely, reliably, and at scale?
That’s where the platform comes in.In the next post, we’ll move from theory to reality and show how this execution layer takes shape across real healthcare workflows.


.png)

