The Tension in Today’s Healthcare System
Over the past two decades, we have digitized nearly every aspect of healthcare. Electronic health records now capture encounters, orders, medications, images, notes, and claims at a scale that was unimaginable a generation ago. We’ve captured nearly every interaction that happens across the care continuum. And yet, despite all of this information, healthcare still struggles to move patients forward efficiently.
You see this everywhere:
- 40%+ of hospital expenses go to administrative overhead.
- 22.5% of physicians spend eight or more hours each week in the EHR after hours.
- Healthcare’s specialized workflows require many purpose-built platforms. Over time, this necessary specialization has created disconnected systems that slow care and exhaust clinicians.
We are at a critical moment in the evolution of healthcare, where it doesn’t suffer from a lack of information, rather it suffers from a lack of systems that do something with that information.
The result is an industry with a data surplus and an action deficit.
The Quiet Failure of Documentation-First Technology
Healthcare technology has been optimized for one thing above all else: recordkeeping.
That focus made sense. Systems of record were a necessary foundation digitizing charts, improving legibility, enabling billing, and supporting regulatory compliance. But documentation, by itself, does not move patients forward.
Other industries learned this lesson years ago. In finance, logistics, and manufacturing, software evolved beyond recording transactions to executing workflows and anticipating outcomes. Healthcare largely did not.
Instead, we layered analytics on top of records and expected insight to magically translate into action. When it didn’t, we compensated by inserting humans everywhere, coordinators, reviewers, navigators, utilization teams, acting as the connective tissue between disconnected systems.
As Atul Gawande once observed, medicine has become a complex system that still depends on heroics. This observation remains painfully current.
A Framework for a Complex Problem
Across industries, modern software tends to follow a familiar progression:
- Systems of Record capture what happened
- Systems of Automation execute what should happen next
- Systems of Intelligence anticipate what will happen
Healthcare, for the most part, is still stuck at the first step. This is not because clinicians resist change or organizations lack data. It’s because the middle, automation system, was never built systematically into the healthcare stack.
That’s why workflows break down despite clean data. That’s why analytics rarely make it to the last mile. And that’s why human decision gates exist everywhere not because humans are better, but because the system can’t act without them.
The Three Pillars of Autonomous Healthcare Systems
Systems of record, automation, and intelligence are interacting elements. Each depends on the others to function in real time. Intelligence without automation is advisory. Automation without intelligence is brittle. Records without either are inert. Autonomy emerges only when all three work together.Closing the gap between data and action requires three capabilities working together.
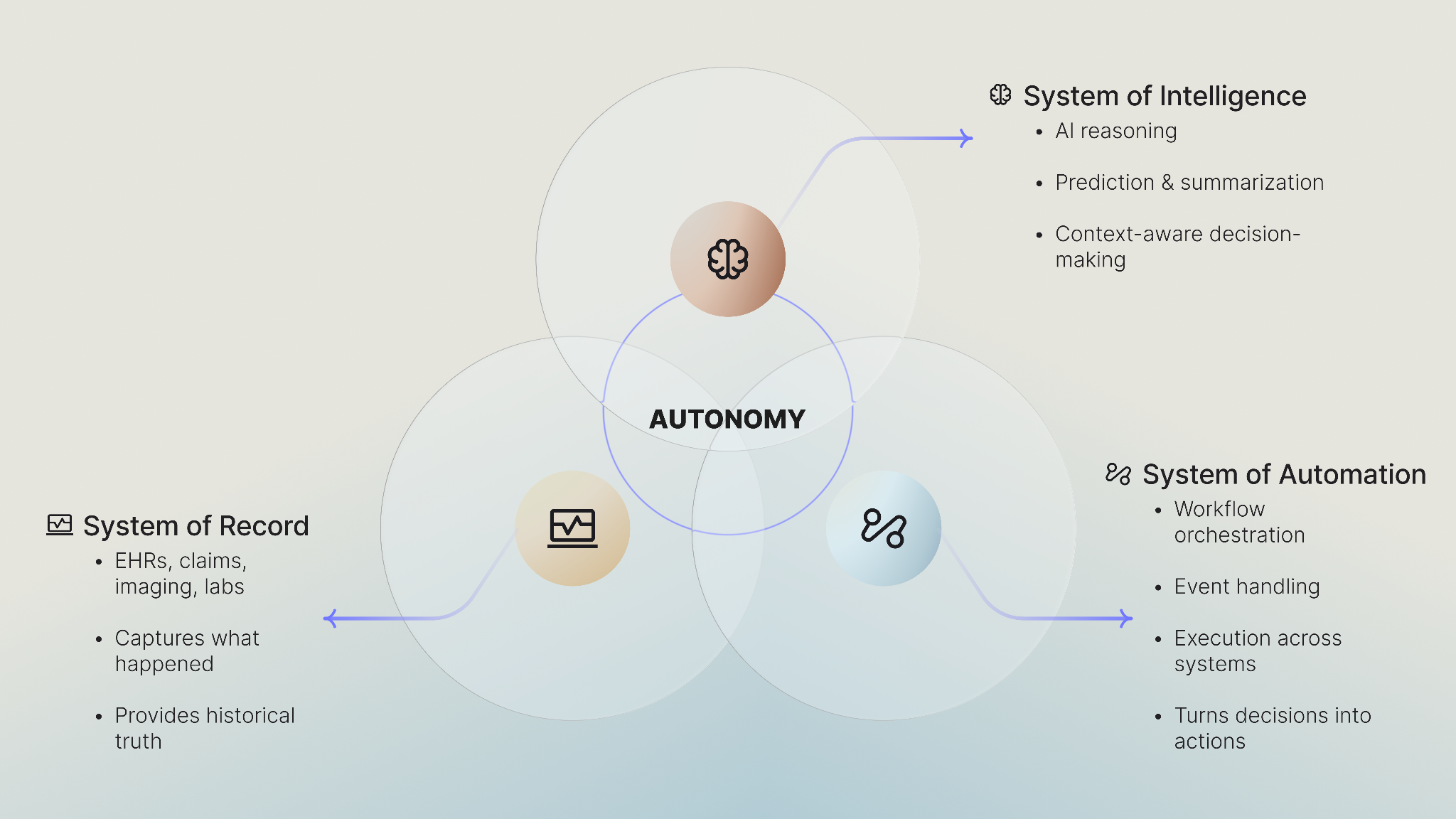
1. Systems of Record: Necessary, But Not Sufficient
Systems of record remain foundational. They provide the historical truth of what happened. But on their own, they don’t move care forward.
- They don’t coordinate teams.
- They don’t close loops.
- They don’t anticipate friction.
They need automation and intelligence to become operational.
2. Systems of Automation: Turning Decisions into Outcomes
Automation is the execution layer that turns decisions into outcomes. Healthcare has invested heavily in record keeping. We are seeing it invest even more in intelligence.
What it hasn’t invested in, at least not systematically, is a System of Automation.This is not scripting or RPA bolted onto legacy workflows. True automation is :
- Listening to events across the healthcare stack
- Orchestrating workflows across EHRs, payers, labs, and patient-facing systems
- Generating tasks, documentation, and communications automatically
- Enforcing guardrails, escalation paths, and human override where appropriate
This is the missing connective tissue in healthcare. Without it, intelligence remains theoretical.
In our experience, automation is also the hardest capability to build not because it’s flashy, but because it must operate across data, workflows, governance, and scale simultaneously.
Without it, AI remains advisory. With it, AI becomes operational. This distinction matters because a system of intelligence without a system of automation is just a recommendation engine. And healthcare doesn’t need more recommendations, it needs systems that act.
3. Systems of Intelligence: Understanding Context, Not Just Language
Intelligence is where decision-making lives. In healthcare, that means the system must understand context:
- What does this patient need next?
- What will the payer require to approve faster?
- What will the PCP need to get their tasks done quicker?
- What risk or gap should be addressed now, not later?
This is where AI models and predictive analytics live. But intelligence alone doesn’t create impact. A recommendation that can’t be executed safely is just another alert.
When These Systems Compound: Autonomy Emerges
Autonomy is not a feature. It’s an architectural outcome. It’s what happens when decision making, and automation compound:
- Routine processes safely run without human intervention
- Humans handle exceptions, not defaults
- Systems learn and adapt over time
Consider patient navigation:
- Today: Manual outreach, static workflows, delayed follow-ups
- With autonomy: Proactive engagement, intelligent triage, continuous orchestration across the care journey
Or operational workflows:
- Today: Manual medication reviews and renewals
- With autonomy: Intelligent review, automated eligibility checks, policy enforcement, and proactive clinician escalation
Autonomy doesn’t replace clinicians, it replaces waiting. And that’s where real ROI comes from, not better dashboards, but faster, cleaner execution.
A Shift in How We Think About Healthcare Software
Autonomous systems invert the traditional model:
- The system acts within predefined boundaries
- Humans intervene when something falls outside those boundaries
This isn’t about removing humans from care. It’s about reserving human judgment for decisions that require accountability, nuance, and clinical context, while letting software handle the rest.
In our own belief, autonomy doesn’t eliminate oversight. It makes oversight intentional. This realization shaped how we built our platform: as a system of automation that enables real-time decision-making to translate into action. Merlin, our unified voice-enabled AI assistant, is one expression of that intelligence but the architecture is designed to support many intelligent applications operating within the same automated foundation.
What Comes Next
Autonomous systems unlock a different future:
- Adaptive workflows instead of static ones
- Personalized patient journeys at scale
- Operational systems that self-correct instead of breaking
But achieving this requires rethinking the healthcare stack, not as a hierarchy, but as an interaction between records, automation, and intelligence.
That architectural shift is what enables autonomy, and is what separates data-rich organizations from action-rich organizations.
Healthcare doesn’t need more digital paperwork. It needs systems that understand, decide, and act together closing the gap between information, execution, and care


.png)

